Interventional oncology, a new weapon against cancer
As part of the demand for more personalized and less aggressive treatments, interventional oncology represents a major field of innovation for cancer treatment. While it makes it possible both to optimize the diagnosis and to expand the therapeutic arsenal, it faces obstacles in terms of funding and accessibility.
To mark the opening of a high-tech platform dedicated to interventional oncology at the Gustave Roussy Institute, Europe’s leading cancer control centre, Alcimed discusses the opportunities for this rapidly expanding discipline in France, whose development was one of the priorities of the latest French cancer plan 2014-2019.
Interventional oncology, a recent discipline with multiple applications
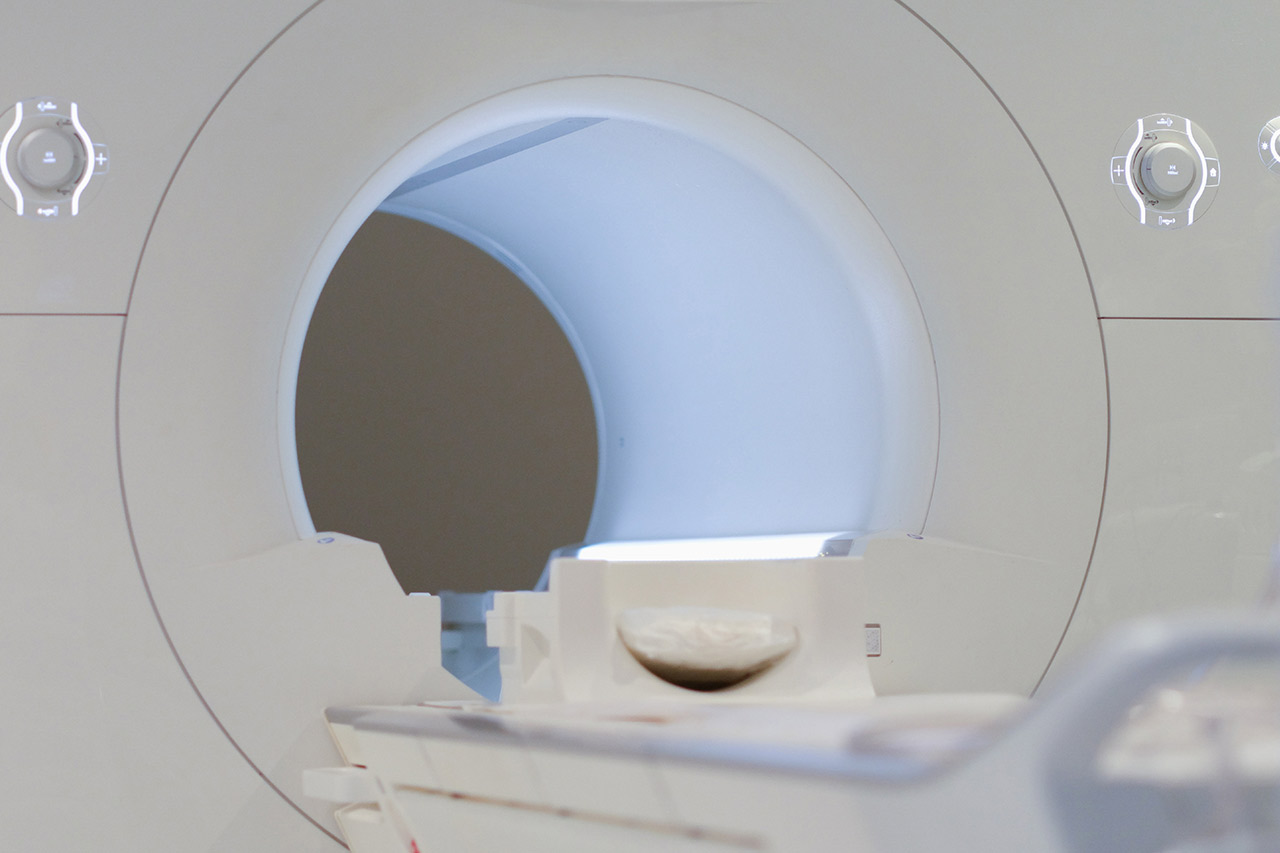
Interventional oncology, a discipline that appeared roughly fifteen years ago, refers to all interventional radiology procedures in oncology. Interventional radiology (IR) is a minimally invasive method for diagnosis or therapy that uses imaging (ultrasound, radiography, fluoroscopy, CT, MRI) and is performed primarily by radiologists. It facilitates the access to a structure inside the body (tumour, blood clot…) by direct transcutaneous route using needles (by choosing a short and safe path), by a natural orifice (urinary system, digestive tract) or by the vascular network after insertion of a catheter. IR is performed approximately 550,000 times per year in France[1].
While IR is well established in certain specialties such as vascular pathologies, interventional oncology is still in its infancy and is now mainly developed in diagnostic procedures. In the era of precision medicine, IR is key in the implementation and evolution of therapeutic protocol: biopsies can be performed with great precision on both superficial and inner tumours using imaging guidance.
Even if they now represent only one third of the procedures, therapeutic interventional oncology procedures are on the rise and offer increasingly effective solutions. They can be used as a complement to or replacement of traditional therapies. The possibilities are numerous: percutaneous destruction of the tumour with heat (radiofrequency, microwave) or cold (cryotherapy) by inserting needles through the skin, injection of chemotherapy (chemoembolization) or radioactive (radioembolization) treatment into the tumour itself via a catheter. These techniques are generally used when surgery is contraindicated, but are increasingly indicated as a first-line treatment, especially for small and localized tumors. For example, ablation and chemoembolization were included as first-line treatments in the European guidelines for the treatment of hepatocellular carcinoma, a specific type of liver cancer, which is an important sign for the recognition of the discipline.
A “win-win” solution for the patient and the health system
Due to its minimally invasive and targeted nature, interventional oncology has many advantages for the patient compared to traditional surgery. The used procedures often allow for surgery under local anaesthesia and hospitalization is generally of short duration, thus providing greater comfort and safety for the patient. Toxicity to healthy tissues is limited by the targeted nature of the actions, thus reducing side effects. As a result, these minimally invasive procedures are often well supported by patients, with a reduced recovery time.
Managing a patient by using interventional oncology also reduces health care costs compared to conventional therapeutic techniques. For instance, treating pulmonary metastases with radiofrequency under radiological guidance costs insurance providers half as much as conventional surgery. This is due to the fact that the duration of the intervention and recovery are shorter, and care can often be provided on an outpatient basis.
A discipline with a promising future
According to Unicancer’s 2025 prospective study, the development of IR will be one of the major developments in cancer management, as will the development of targeted therapies, immunotherapy and oral therapies. Like the Gustave Roussy Institute, healthcare institutions are opening high-tech technical platforms dedicated to interventional oncology procedures to meet the growing demand.
Thanks to innovations in both imaging equipment and interventional tools, the precision and technique of interventional oncology are constantly improving and its indications are expanding. The therapeutic portfolio of interventional oncology has expanded significantly in recent years with new techniques under evaluation, such as electrochemotherapy or high intensity focused ultrasound. Its use in combination with immunotherapy treatments is under investigation, which could be a promising opportunity for the field. The way it is carried out is also changing thanks to the development of guidance software and the emergence of multi-modal rooms allowing the fusion of images from different imaging equipment. Finally, in the coming years, interventional oncology will increasingly use robotic tools, such as autonomous catheters, artificial intelligence and augmented reality, which are already being used to increase the accuracy of other interventions.
A development slowed down by mainly financial and accessibility obstacles
However, while interventional oncology has clear benefits for both patients and healthcare systems, its actual use remains limited due to a lack of recognition and funding. Interventional oncology is still not visible enough and there is a long way to go before it is fully integrated into the cancer care system. A major challenge is the adaptation of the nationally defined classification of medical interventions (classification commune des actes médicaux, in French) to better promote certain acts and include others that are not yet listed. This requires the implementation of solid, randomized studies, which will make it possible to establish its medico-economic benefits. However, such studies remain difficult to implement due to the multiplicity of procedures and the small number of patients. It is also necessary to adapt the reimbursement of these procedures which use highly sophisticated and expensive equipment. Today, the costs are often significantly higher than the reimbursement via the diagnostic-related group system as the rates per intervention are too low and as there is no separate reimbursement for expensive medical devices. Even if the list of reimbursable services and products has recently been expanded beyond implantable medical devices, certain medical devices used in IR are still not reimbursed. Removing the financial barrier is therefore a major priority to enable the deployment of interventional oncology.
An additional barrier is the accessibility to interventional oncology techniques: they require dedicated operating rooms and trained staff. Today, this offer is very limited in France. Hospitals which provide both costly equipment and the necessary surgical environments are often concentrated in regional metropolitan areas. Therefore, allowing all cancer patients to have access to the therapeutic solutions offered by IR is a major challenge.
“Interventional oncology represents a real innovation for the patient, but its benefits are not sufficiently recognized. It is essential to consider it as a pillar of cancer treatment, to integrate the interventional radiologist into the definition of the patient pathway and to support its development through a evolution of reimbursement” concludes Delphine Bertrem, Head of Alcimed’s Health Business Unit in Paris.
It remains to be seen whether the 2014-2019 cancer plan, aimed at providing a better framework for interventional radiology and an update of the associated regulatory and pricing system, will achieve its objective.
[1] Société Française de Radiologie, Décembre 2016
Do you have an exploration project?
Our explorers are ready to discuss it with you