What are xenotransplantations and xenografts?
Xenotransplantation is the transplantation of organs and tissues from a donor whose biological species is different from that of the recipient. It therefore includes the possibility of transplanting animal organs into human beings. These foreign organs or tissues are called xenografts. Today, pigs are the preferred donor species for humans, due to their ease of rearing and the physiological and morphological similarities between human and pig organs. In addition, their rapid sexual maturity, short gestation period and large litter size make them advantageous.
Graft rejection by the recipient organism is the main challenge
While xenografts appear to offer a promising solution to organ shortage, there are many challenges to overcome before they can replace human organs. The biggest challenge is the immune response of the recipient organism. In the case of human organ donation, the recipient’s negative immune response and the risk of graft rejection are already high, and are now mitigated by the use of immunosuppressive treatments. In the case of pig organ transplants, immunological barriers are much higher, notably due to the presence in human blood of antibodies targeting xenoantigens – antigens external to the organism – and present on the surface of pig cells. The immune reaction is immediate, and the graft is rejected by the human body in a matter of minutes: this is known as “hyper-acute rejection”.
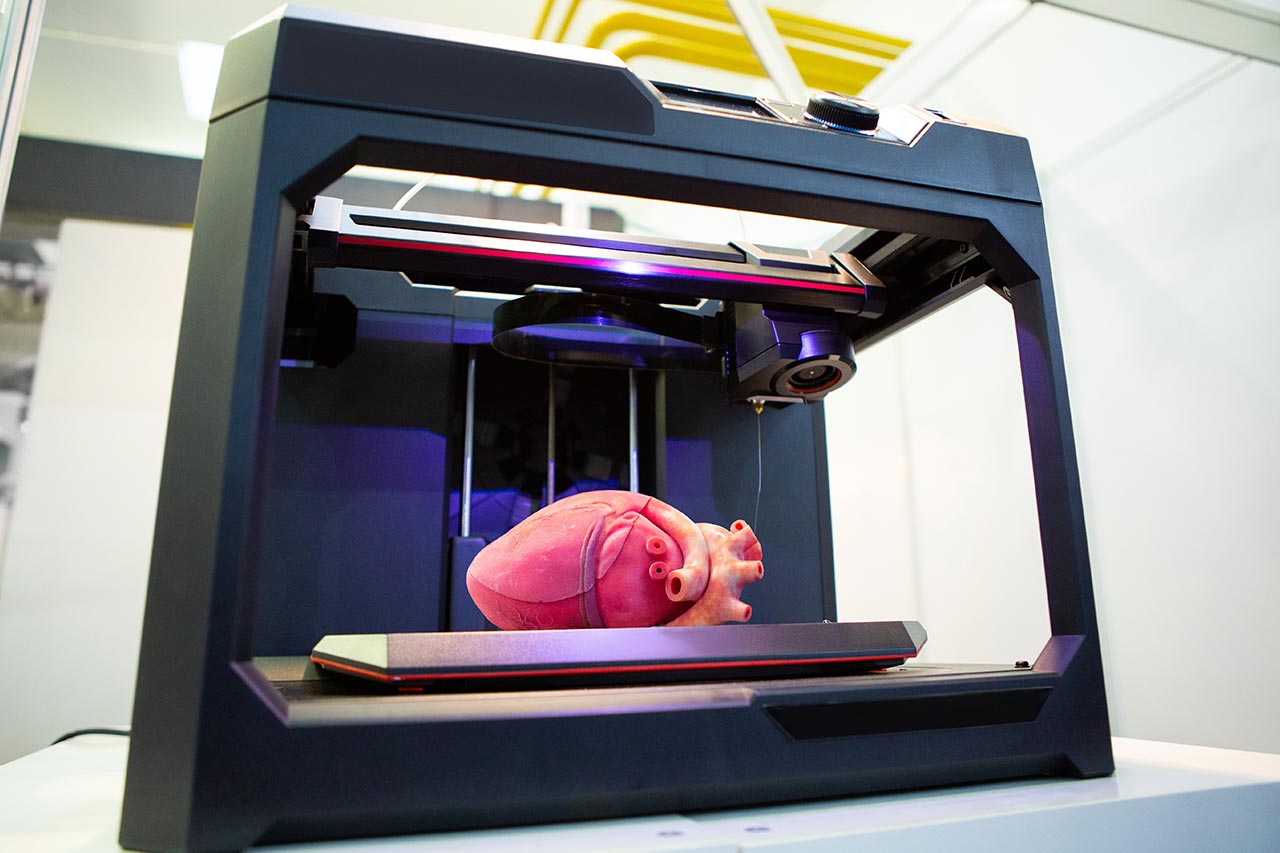
Genetic modification as a solution to prevent xenograft rejection
Recent developments in genome editing, in particular using the CRISPR technique, have made it possible to introduce human genes into the porcine genome in order to increase the likelihood of acceptance of the porcine organ by the human organism. Several dozen genetic modifications have been attempted, with some specific porcine genes deleted. These modifications have resulted in promising pre-clinical models with high survival rates.
Learn more about how our team can support you in your projects related to genome editing >
The first xenografts on brain-dead human recipients took place in 2021 in the USA, using genetically modified pig kidneys. While examination of the pig transplants revealed inflammatory cells as a sign of rejection, these had the same molecular signature as when they are found against a human graft. These were inflammatory cells expressing typical rejection genes, suggesting that anti-rejection treatments already available for human grafts could be tested in xenotransplantation. In addition, these trials made it possible to optimize genetically modified pig models. Since these initial trials, several kidney transplants have been carried out in the USA at NYU Langone Health, with no obvious signs of rejection and survival times of several weeks.
American biotech Revivicor is also developing genetically-modified pig transplants, including a pig heart transplanted in January 2022 into a patient suffering from heart failure and condemned to die without a transplant. The patient survived for 2 months before dying, but no signs of rejection were detected. However, autopsy of the transplanted porcine heart revealed the presence of porcine cytomegalovirus (pCMV). After the risk of “hyper-acute rejection”, the risk of zoonosis is the second major medical risk associated with xenografts. Solutions to this problem are already under study! For example, British biotech eGenesis is developing a platform, EGEN, to address these two major risks.
Recent developments in xenotransplantation have overcome one of the major barriers to transplantation – hyperacute rejection – and confirmed the potential of the genome-editing approach. Nevertheless, many other challenges surround xenografts, such as zoonoses. In addition, there are ethical issues surrounding animal welfare, transgenic animals, and the question of species boundaries, all of which need to be carefully addressed. Finally, the development of an appropriate regulatory framework to ensure patient safety will have to be developed.
At Alcimed, we’d be delighted to accompany you on this uncharted territory and continue exploring this promising subject! Please do not hesitate to contact our team.
About the author,
Diane, Project Manager in Alcimed’s Life Sciences team in Germany